Aerospace medicine: A General Outlook
Have you ever wondered what type of physician backs the American space program? Who keeps an eye on the astronauts’ health and safety while they are stcoralblueoutlet kleankanteentrinkflasche moorecains tatascarpe saldigeox relaxdaysstore senzamai blundstoneprezzi donkeyluckycat geoxoutlet 24bottlesclima donkeyluckycat cainsmooredonna saldibenetton uspoloassnscarpeationed in space and is on standby for when they go and return? Who, in addition to engineers, pilots, and other top experts, contributes to the planning of the planned Lunar and Mars missions? Aerospace medicine is this area of study.
Clinical care, research, and operational support for the health, safety, and performance of the crew and passengers of aircraft and spacecraft, as well as the support staff who help operate such vehicles, are the main areas of focus in aerospace medicine. This group frequently works and lives in physically and psychologically demanding circumstances in distant, severe, or enclosed places. Practitioners aim for the best human-machine compatibility in work environments that are full of engineering safeguards against environmental risks.
A brief history:
- 1783: Jean-Francois Pilâtre de Rozier and Marquis d’Arlandes make the first manned free balloon flight.
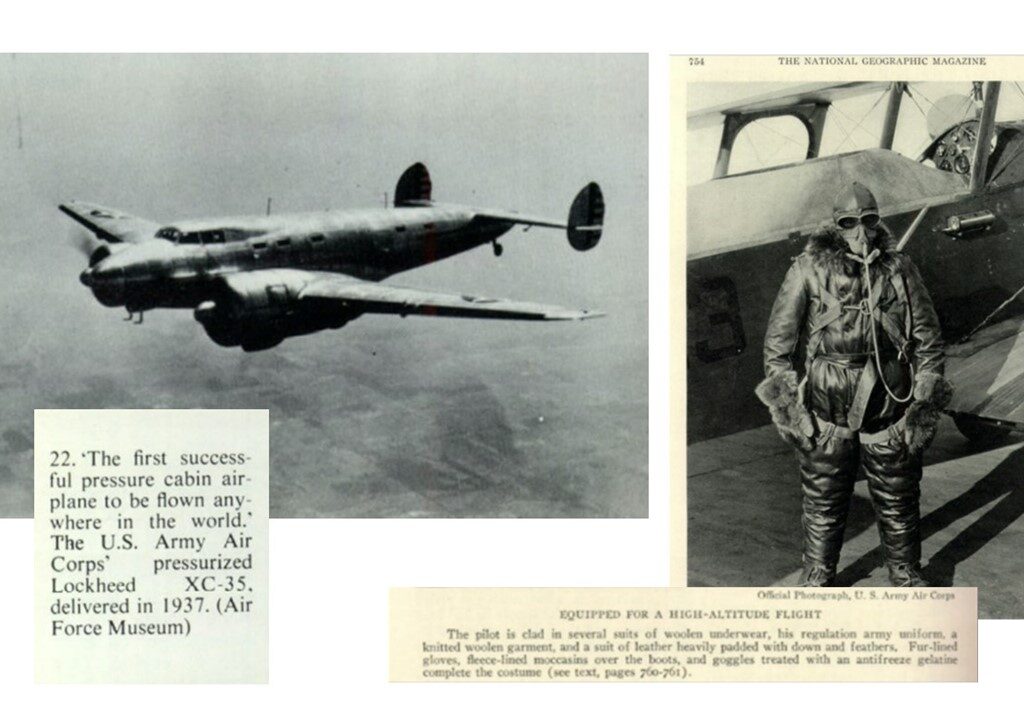
- 1875: French scientists Gaston Tissandier Joseph Croce-Spinelli and Théodore Sivel reach an altitude of 28,000 ft in their balloon using oxygen in sheepskin bags provided by physiologist Paul Bert.
- 1911: Lt. Washington Irving Chambers meets with aviation pioneer Glenn Curtiss to discuss the possibility of aircraft aboard Navy ships. Dr. Ralph P. Greene was the first U.S. medical officer ordered to fly duty. Greene later serves as the 2nd president of the Aerospace Medical Association.
- Army Flight Surgeon Col. Isaac H. Jones (1881–1956) published his book Equilibrium and Vertigo.
- 1922: Five U.S. Navy lieutenants graduate from the School of Aviation Medicine as flight surgeons.
- 1925: The Air Corps Physiologic Research Laboratory at Wright Field, Dayton, OH, investigates hypobaric states, hypoxia, and the effects of centrifugal force on pilots.
- Lieutenant Bertram Groesbeck Jr. (1894–1968) is the first medical officer in the U.S. Navy to be given wings as a Naval Aviator. He writes an essay about “blind flying” (instrument flight) in 1930 and publishes it in the Journal of Aviation Medicine.
- In 1939 the U.S. Navy establishes its School of Aviation Medicine at Pensacola; FL. On November 30, five naval flight surgeons received their diplomas.
- Lt. Col. (Dr.) William R. Lovelace makes the first aircraft flight using pressure breathing in 1942.
- 1964: The Coriolis Acceleration Platform and Vestibular Unit are dedicated at the U.S. Navy School of Aviation Medicine.
- 1995: Developed by Navy Flight Surgeon Capt. Angus Rupert, the Tactile Situation Awareness System (TSAS) shows promise in mitigating spatial disorientation in flight.
Effects of Space on the Body
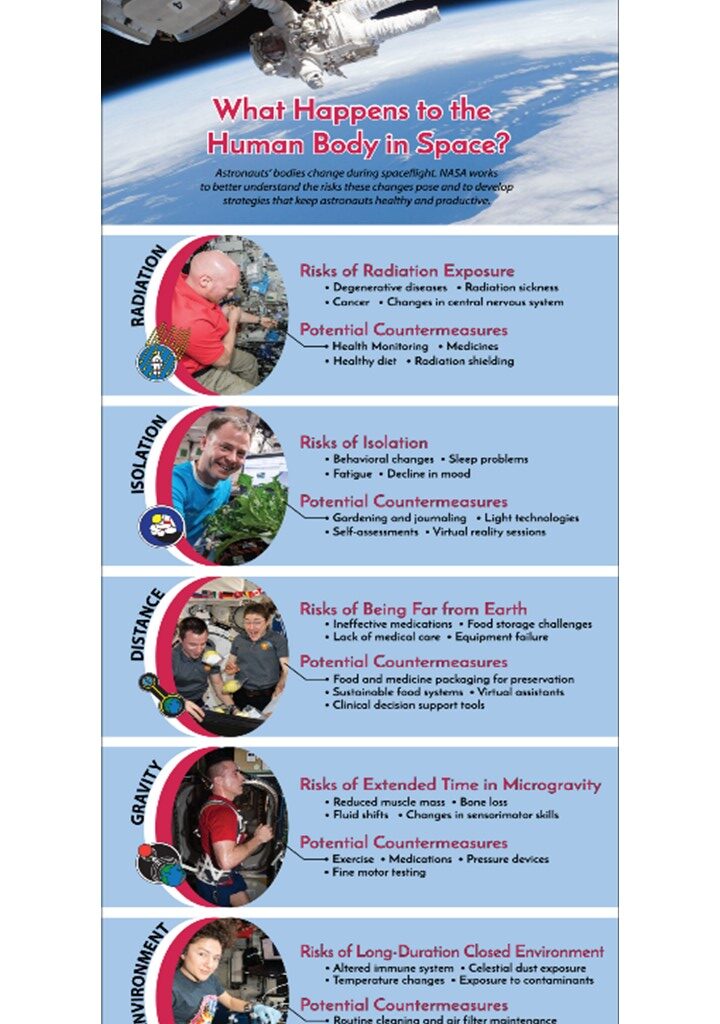
The short- and long-term impacts of space conditions on the human body have been researched by space agencies. When they suffer from ailments like altitude sickness or the sensation of their ears “popping,” passengers provide the general public a brief glimpse into the impacts of flight. As soon as people leave the safe bubble of our atmosphere, several risks arise, making life in space considerably more challenging. According to NASA, there are five types of stress associated with space travel. These can be summarized with the acronym RIDGE:
- Radiation from space: Astronauts are exposed to 10 times as much radiation aboard the International Space Station as they are on Earth. This poses a higher chance of developing cancer and might harm the central nervous system, which could lead to issues with cognition, movement, and behavioral abnormalities. Radiation illness and degenerative tissue disorders, including cataracts and heart problems, can also be brought on by space travel.
- Isolation and separation: Living on the International Space Station (ISS) or a spacecraft has psychological effects in addition to physical ones, which are equally significant. Long-term confinement in a limited area can lead to behavioral problems in the group as well as a drop in mood and morale, difficulties sleeping, and boredom.
- Distance from Earth: It’s not precisely possible for an astronaut to dial 911 and request an ambulance to take them to the hospital if they become ill or hurt. They pose a health concern just by being so distant from Earth. This is a problem on the ISS, but it will be crucial for upcoming Moon and Mars missions.
- Gravity fields: The absence of gravity has an impact on balance, locomotion, head-eye and hand-eye coordination, and spatial orientation. Additionally, without gravity, your bones lose minerals, resulting in a monthly density loss of nearly 1%. To combat this, astronauts must spend 2.5 hours every day working out in space.
- Enclosed and Hostile conditions: Living a sheltered life is unhealthy. Your immune system is weakened, germs may spread readily, and stress hormones are increased.
Modern trends in aerospace medicine:
Aerospace medicine is regarded as a specialist area of medicine that is concerned with the upkeep of the health and effectiveness of the aircrew in the environment of space and flight. Additionally boosting the global aerospace medicine market’s revenue growth is the pharmaceutical industry’s growing interest in aerospace medicine. Doctors in aerospace medicine work for commercial airlines, the military, space agencies, regulatory organizations, and independent clinics that specialize in medical flight certification.
When people are subjected to the challenges of aircraft flight, such as high temperatures, low oxygen levels, atmospheric pressure, noise, radiation, and powerful acceleration and deceleration forces, aerospace medicine supports their safety and effectiveness. Aircraft medicine, often known as aviation medicine, plays a significant role in ensuring that the aerospace environment is safe and healthy for every pilot. But aerospace medicine is a brand-new, cutting-edge area of medicine that opens up a ton of business prospects for drug manufacturers and other suppliers.
The Aerospace Medical Association (AsMA) conducts several case studies and investigations on aviation, space, and environmental medicine on modern trends. The man-machine interaction has been significantly altered by evolving technology and unmanned aerial vehicles, leading to a shift in the practice of aerospace medicine. The worldwide aerospace medicine market is anticipated to increase as a result of the expanding airline sector and military aviation forces. Aerospace doctors are knowledgeable about the physiological effects of exposure to the space environment and appropriate medical care to guarantee everyone’s safety in the sky. The expansion of the aerospace medicine industry may be hampered by the high quantity of harmful chemicals found during the flight.
Flight surgeons are medical professionals with specialized training in aircraft medicine. There are medical professionals in aerospace medicine throughout the world. The aforementioned problems are not sufficiently covered in primary care or surgical specializations to treat the medical needs of military and civilian aviators and space travelers. Aerospace medicine is growing more and more appealing with the rise of passengers of all ages. Soon, it is anticipated that the “Aerospace Medicine Market” would rise astonishingly. AsMA is committed to improving the performance, safety, and health of everyone who travels or works in the air, underwater, or in space.
Visit: https://www.nasa.gov/sites/default/files/atoms/files/space_portal_graham_mackintosh.pdf
Future of Aerospace medicine
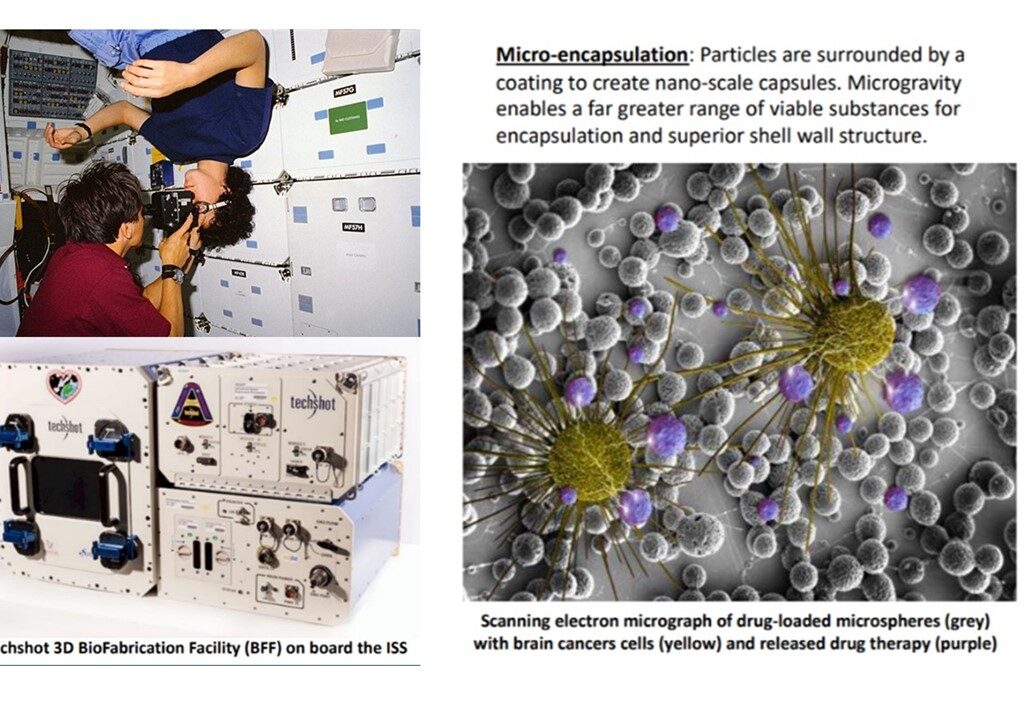
The previous year has demonstrated that medicine and medical treatments aren’t just limited to doctor’s offices. Telemedicine and AI technologies helped to guarantee that individuals received the care they required even while a pandemic swept the planet. Future medicine might be more intelligent. From the comfort of our homes, we could examine our blood for infections. We could find a tap and transform tap water into sterile IV fluid instead of rushing a dehydrated patient to the hospital. Medical imaging devices might scan our bodies whenever and wherever we are and transmit automatic readouts to human and artificial intelligence (AI) medical professionals anywhere in the world (or worlds). That is the hope for the future of Earth. However, it is already underway in space, hundreds of miles above the surface, where aerospace medicine is creating the foundation for tomorrow’s healthcare.
Awareness among medical students:
Specific training concentrating on the medical fields like space medicine receives less attention. Medical students’ education can help them become candidates or educators in space medicine, and this education may be required for the next generations. In the current study, we sought to gauge the degree of knowledge in this area among Turkish medical school students. Resources and Method: Our research is intended to be cross-sectional and includes medical students. Participants in various grades who consented to complete the space medicine-focused awareness questionnaire were included. It was shown that 42.1% of the students lacked knowledge about space medicine. Similarly, 56.3% of the students who took part in the survey were not aware that this specialty was within the umbrella of medicine. The majority of medical school students were unaware that there was a discipline of aerospace medicine, and only a small percentage of them had any understanding of space medicine.(Emre, 2022)
Aerospace medicine and Sri Lanka: A Pioneer.
Dr. (Mrs.) Anoma Jayasinghe, Group Medical Officer of Sri Lankan Airlines, has become the first Sri Lankan professional in aviation medicine to be selected as a Member of the International Academy of Aviation and Space Medicine (IAASM), in recognition of her contribution to this field in Sri Lanka for over a decade. She is a full member of the Australian Society of Aerospace Medicine, a Member of the Aero Space Medical Association USA (AsMA), and a Designated Aviation Medical Examiner of the Civil Aviation Safety Authority Australia (CASA).
Dr. Jayasinghe would be an Academician of IAASM, Academicians are leaders in aerospace medicine and related sciences who work as a select group and provide a platform for academics and medical professionals to present original scientific papers related to aviation and space medicine.
Founded in 1955, IAASM (www.iaasm.org) has a limited membership of approximately 240 medical professionals from around the world, from airlines, civil aviation regulatory authorities, and organizations involved in aviation and space travel, the national carrier said in a media release. She pursued post-graduate training in Aviation Medicine and obtained the Australian Certificate of Civil Aviation Medicine from Monash University; Aviation Medicine Course from Singapore Aviation Academy; and a Diploma in Occupational Health and Safety from the University of Colombo. Aviation and Space Medicine are the fields in medicine that are concerned with the maintenance of health, safety, and performance of those involved in aviation or space activity.
Reference list:
AsMA | Aerospace Medical Association (no date) www.asma.org. Available at: https://www.asma.org/about-asma/careers/aerospace-medicine .
Dr. Anoma Jayasinghe, first Sri Lankan member of prestigious IAASM (2017) The Sunday Times Sri Lanka. Available at: https://www.sundaytimes.lk/170312/business-times/dr-anoma-jayasinghe-first-sri-lankan-member-of-prestigious-iaasm-232034.html (Accessed: 5 July 2022).
Emre, S. (2022) What Do Medical Students Know About Space Medicine?
Gifford, S. (2021) Future Aerospace Medicine: Coming to a Planet Near You, Now. Powered by Northrop Grumman. Available at: https://now.northropgrumman.com/future-aerospace-medicine-coming-to-a-planet-near-you/ .
McSweeney, K. (2021) The Next Frontier: Aerospace Medicine, Now. Powered by Northrop Grumman. Available at: https://now.northropgrumman.com/the-next-frontier-aerospace-medicine/ .
Singh, A. (2022) Aerospace Medicine Market 2022 Industry Trends, Sales, Supply, Demand, Analysis & Forecast to 2031, EIN News. Available at: https://www.einnews.com/pr_news/566470136/aerospace-medicine-market-2022-industry-trends-sales-supply-demand-analysis-forecast-to-2031 (Accessed: 5 July 2022).
Stratton, E. (2019) Aerospace Medicine? www.emra.org. Available at: https://www.emra.org/emresident/article/aerospace-medicine/ .
Tarver, W.J. (2007) An Introduction to the History of Aerospace Medicine, ntrs.nasa.gov. Available at: https://ntrs.nasa.gov/citations/20070029992 (Accessed: 5 July 2022).
Image Credits: